TIVA – a helpful guide to get you started… (7 mins read)
Introduction:
Total Intravenous Anaesthesia is a concept I’m familiar with through my FRCA study, and some exposure within clinical practice, however I have found that use of TIVA is variable from department to department and if you’re not working in a very pro-TIVA environment, then chances are you’ll have fairly limited exposure to it!
I’ve written this blog post for 3 main reasons:
1. My current department is very pro-TIVA and hence I’d like to get good at it myself! The only way to do so is to understand TIVA principles, and apply these to daily practice!
2. It is becoming increasingly popular, and many anaesthetists in training are still unfamiliar with it. Lack of training and competence is a recognised contributory factor in cases of accidental awareness with TIVA in NAP 5. [1]
3. It can easily be asked in an exam setting – weather it’s the Primary FRCA or the Final FRCA!
For the purposes of this blog post I will be focusing on TIVA for adults using propofol, and TCI models of administration.
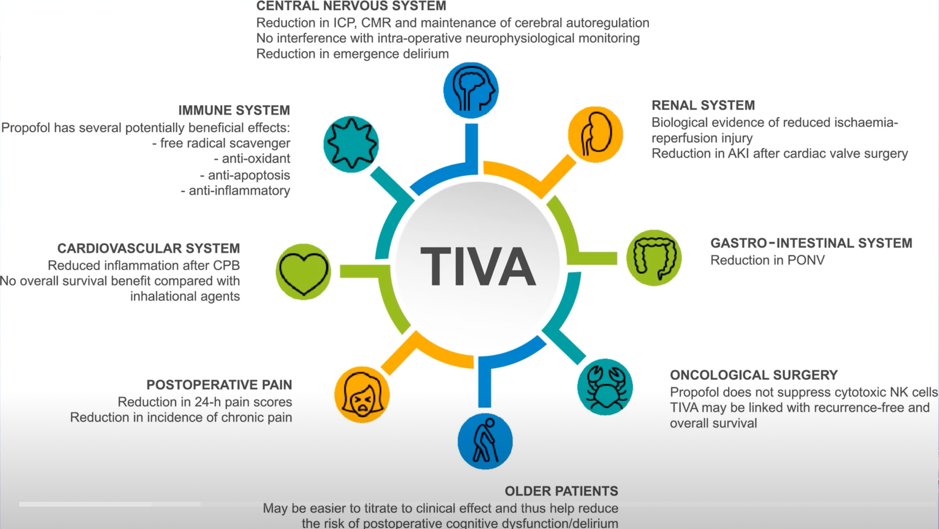
Let’s start with potential benefits:
The following infographic summarises the benefits to the patient extremely well [2]
And let’s not forget the huge benefits to the environment!
Possible indications for TIVA:
1. When inhalational anaesthesia is not possible:
a. Outside of theatre
b. Transfer
c. Some airway operations
d. When intra-operative monitoring of somatosensory & motor evoked potentials is required
e. MH
2. High risk of PONV
3. Anaesthetist preference
TIVA in practice:[3]
Administering TIVA can be done in two ways:
1. Manual dosing – giving a bolus and setting an infusion rate (ml/hr)
2. Target controlled Infusion (TCI) – this is the preferred and recommended option and this is what I’ll be discussing in further detail below.
Understanding the pharmacokinetic principles and models:
Background:
· A TCI pump contains a micropressor programmed with pharmacokinetic models for relevant drugs
· Most models have been developed in young, health, non-obese subjects (which is why they will have a max weight limit, and caution is required when administering TIVA to older, obese and/or critically unwell patients)
o Remember plasma drug concentrations in individual patients are very rarely going to be exactly the same as those predicted by the models!
· This is why clinical judgement and using meticulous monitoring is equally as important.
o Titrate to clinical effect
o Use pEEG especially when using a NMB.
· NAP 5 highlighted that the 2 most commonest causes of accidental awareness during TIVA were:
o 1. Failure to deliver the intended dose od drug
o 2. Poor understanding of the underlying pharmacological principles.
So how do you administer TIVA safely in 3 easy steps!
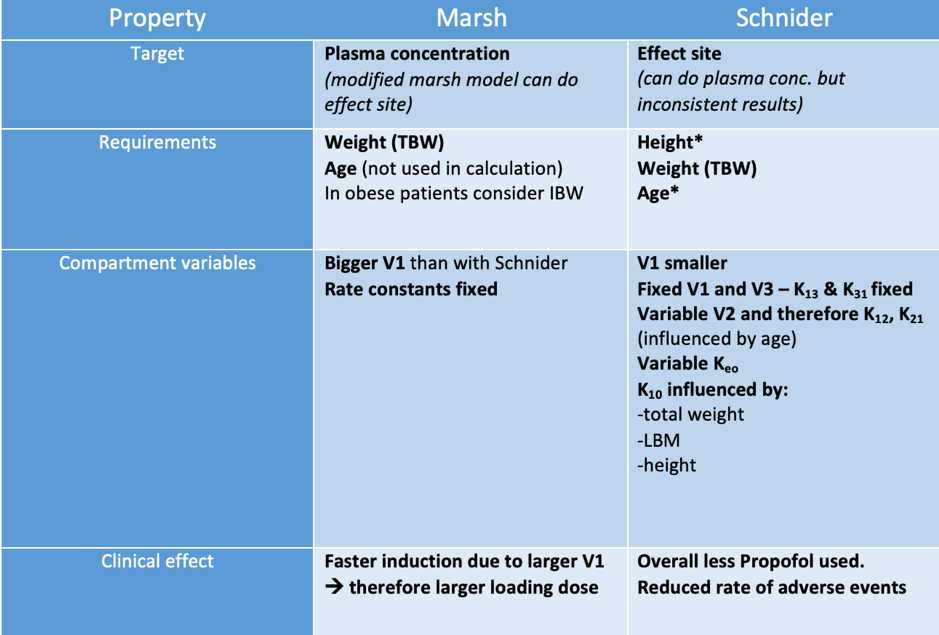
Step 1: Choose the right model:
Adults:
1. Marsh
2. Schnider
3. Eleveld*
Paediatrics:
1. Kataria – 3-16 years. 15-61kg
2. Paedfusor – 1-16 years. 5-61kg
3. Marsh – Teenagers >61kg
4. Eleveld*
*Eleveld is a newer model that I have not had the chance to use yet but definitely seemed to be the latest “IT” model in the world of TIVA at the recent Association of Anaesthetists TIVA webinar as it can be used for obese patients, paediatrics and adults.
Short answer – Generally departments are familiar with one model more than the other. Pick one, and practise getting used to it first.
If you have a TIVA enthusiast within your department, pick their brains and find out why they prefer one model over the other!
Long answer: Having an understanding of each different pharmacokinetic model, its advantages and limitations in relation to your patient will help you decide!
Here’s a helpful table to get you going:
Step 2: Choosing the right induction target drug concentration for a patient
The drug concentration achieved should be sufficient to produce:
1. Loss of consciousness (LOC)
2. Prevent movement in response to painful stimuli
Careful balance is required as too high of a concentration can result in serious side effects such as marked hypotension and/or delayed recovery from anaesthesia.
Starting concentrations should be chosen depending on 3 main factors:
1. Patient characteristics
2. Co-administered drugs
3. Clinical situation
How to choose the right induction dose? (for adults only)
Induction – Propofol 1% TCI - typically 4-6 ug.ml-1
Tips:
1. For generally fit and well patients (using Schnider), I programme my induction dose concentration to the “bolus” dose I would usually give when manually administering – this will appear on your TIVA pump screen when programming your concentration dose.
2. For elderly/critically unwell patients it may be wiser to “start low, and go slow” – as you can titrate the dose to clinical effect and is associated with less severe, rapid falls in blood pressure.
Step 3: Choosing the right maintenance dose for a patient
Maintenance dosing is influenced by:
1. Magnitude of surgical stimulus
2. Co-administered - see below
3. Patient characteristics – e.g. higher doses required in ‘anxious’ patients and lower in older, frail, unwell patients
Co-administered drugs:
· Reduced Propofol requirements with:
· Opioids – synergistic effect
Remifentanil can reduce Propofol requirements by approx. 50%!*
· Regional anaesthesia – decreased response to noxious stimuli
· Other drugs which can influence dosing:
· Benzodiazepines
· Ketamine
· Alpha-2 adrenoreceptor agonists – clonidine
· Magnesium sulphate
· Nitrous oxide
How to choose the right maintenance dose? (for adults only)
Maintenance – Propofol 1% TCI typically:
3-6 ug.ml-1 without opioids
2.5 – 4 ug.ml-1 with opioids
Tips:
Observe:
1. Concentration at which when patient:
a. Loses consciousness
b. Loses response to painful stimuli – this can be helpful in determining the ‘maintenance’ concentration.
2. Clinical signs of awareness
3. pEEG monitoring if using
*Propofol + Remifentanil
Remifentanil can reduce Propofol requirements by approx. 50%!
However, remember Remifentanil is still an analgesic and Propofol is still a hypnotic and it is important not to confuse the two, particularly at induction.
Safety aspects of TIVA:[3]
I have classified these to aid memorising the extensive list! Hopefully this will help you in exam situations as well as your clinical practice!
Drugs:
Preferable to stock only 1 concentration of Propofol
Remifentanil should be diluted to a single standard concentration
Equipment:
Syringes:
Use single brand of syringes – as syringes with the same capacity can have different internal diameters therefore influencing the degree of “push” and therefore volume being delivered to the patient
Ampoule neck or rubber stopper should be disinfected with alcohol wipe prior to drawing up drugs
Drug labels only attached AFTER drug is drawn up
Syringes should have luer lock connectors to reduce the risk of accidental disconnection
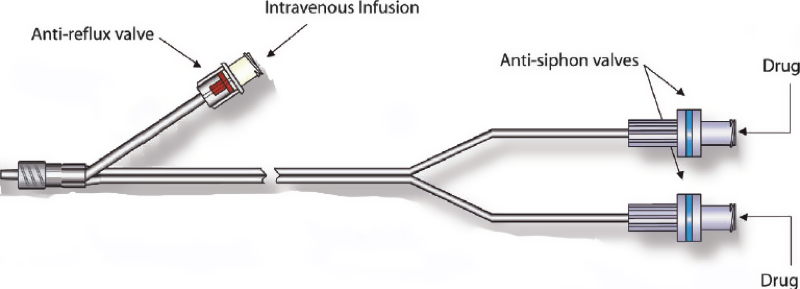
Infusion giving sets:
Preferable to have designated TIVA sets with:
Luer Lock connectors at each end
Anti-siphon valve on the drug deliver line(s) – to prevent uncontrolled infusion from a damaged syringe
Anti-reflux valve on any fluid administration line - to prevent back-flow of the drug up the infusion tubing
Drug and fluid lines should join together as close to the patient as possible to minimise dead space in which a drug can accumulate rather than entering the vein.
Limit number potential sites for leakage - additional connections/3 way taps
IV cannula:
Secure
Visible wherever possible
Inspect site immediately if patients’ response to the infused drug (s) appears less than would be expected
Pumps:
Adequate numbers of TCI pumps should be available
Preferable to use a single model of TCI with a locally approved set of pharmacokinetic models
Advisable to have standard lay out of drugs in pumps
Pump(s) should be visible throughout anaesthesia
Visual display of infusion in progress
Audible alarms – high pressure, stopped infusion, empty syringe, disconnection from mains, low battery
Charge before use
Use mains power where possible to prevent failure secondary to battery depletion
Regular equipment checks with policy in place in case of failure
Should not use infusion pumps that automatically decrease the infusion rate to a low “keep vein open – KVO” when the syringe is nearly empty
Monitoring:
Standard Association of Anaesthetists (AAGBI) monitoring
pEEG monitors should be available in adequate numbers in areas where TIVA is in use.
Conduct:
Checks BEFORE starting TIVA
o Drug to be administered
o Programming
o Infusion set
o IV cannula
o Monitoring on
NMB should only be given after LOC
pEEG should start BEFORE administration of NMB
All IV sites used for TIVA should be flushed at the end of the procedure
10 AAGBI recommendations:
1. All anaesthetists should be trained and competent in the delivery of TIVA
2. When using TIVA for maintenance of General Anaesthesia – TCI is recommended
3. Starting concentrations should be chosen depending on 3 main factors:
a. Patient characteristics
b. Co-administred drugs
c. Clinical situation
4. It is preferable to stock only one concentration of Propofol and to standardise dilution concentrations of remifentanil.
5. Specific infusion sets designed for TIVA are recommended. Infusion sets used for TIVA should have:
a. Luer Lock connectors at each end
b. Anti-siphon valve on the drug deliver line (s)
c. Anti-reflux valve on any fluid administration line
6. Infusion pumps should be programmed only AFTER the syringe containing the drug to be infused has been placed in the pump.
7. IV cannula through which TIVA is being administered should ideally be visible throughout.
8. Anaesthetists should be familiar with the principles, interpretations and limitations of processed EEG monitoring.
9. Processed EEG (pEEG) monitoring is recommended when a neuromuscular blocking (NMB) drug is used with TIVA.
10. The same standards of practice and monitoring apply regardless of the location of where anaesthesia is taking place. E.g. MRI
Take home points:
1. TIVA has many potential benefits and it is important for anaesthetists to be equally competent in intravenous anaesthesia as they are with inhalational anaesthesia
2. Having an understanding of the pharmacokinetic principles and pharmacodynamic effects of different TIVA drugs as well as different co-administration drugs will help you select the safest doses for induction and maintenance.
3. Remember to consider the patient as a whole – age, clinical status, co-administration drugs, type of surgery
4. Always use pEEG when using TIVA with a NMB
5. Get practising! The only way to get good at it is to get stuck in, so have a chat with your supervising consultant on your next case! Setting up really doesn’t take as long as you think…
References:
1. NAP 5 audit report - https://www.nationalauditprojects.org.uk/NAP5report
2. AAGBI – TIVA webinar – (last accessed 30.09.2021)
3. AAGBI Guidelines for the safe practice of total intravenous anaesthesia (TIVA) 2018 doi:10.1111/anae.14428