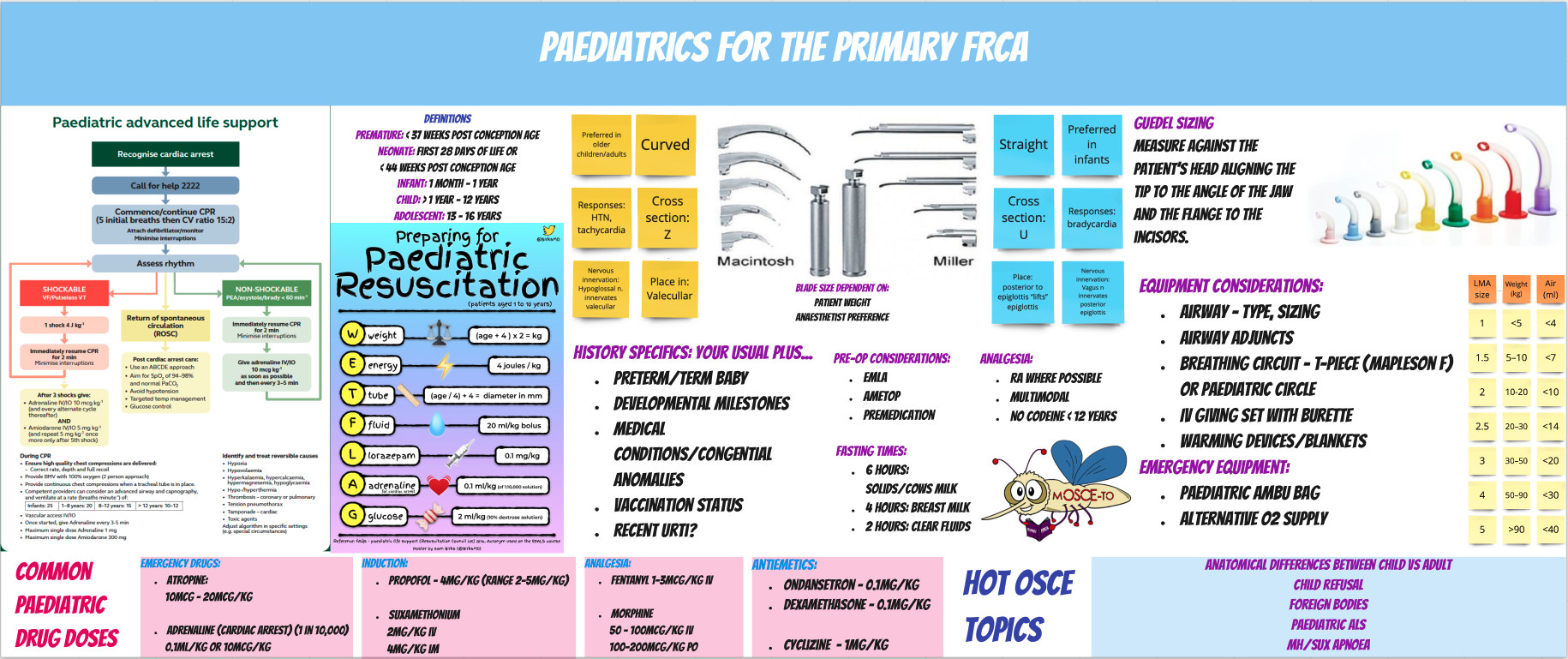
Practical Paediatrics for the Primary FRCA (5 minute read)
This week’s blog posted is all about Paediatrics for the Primary FRCA.
I’ve put together an infographic which contains an overview of paediatrics, the things you need to know and some essential doses and calculations you can always refer back to!
I’ll discuss some more practical considerations in a little more detail below.
Practical considerations:
Recent URTI?
Postpone or proceed?
Take into consideration any ?COVID symptoms, other presenting symptoms, type of surgery and its urgency, the child’s age and comorbidities.
· <1 year – generally a lower threshold to cancel because the risk of respiratory complications is higher
· >1 year – if the child is clinically appears well with very limited symptoms (such as only clear nasal discharge) with no other symptoms, is not requiring intubation for the proposed surgery and the surgery itself does not involve the airway then it may be reasonable to proceed with the case. ALWAYS discuss with a senior – it should be a shared decision making approach involving yourself, the parent, the consultant anaesthetist and surgeon!
· Warning signs include - purulent nasal discharge, productive cough/fever, signs of LRTI involvement – desaturation, wheeze à the case should be postponed for at least 4 weeks where possible.
Airway Management:
Intubation
• All infants less than 5 kg or under 44 weeks gestational age should be intubated.
• Straight blades (Robertshaw or Miller): use in neonates and infants (large floppy epiglottis – blade helps to move it out of the way)
• Curved blade: easier to use once the child is 6–10 kg.
· Type of ETT – most textbooks will state uncuffed especially for children aged 1-10 years, however in practice we now use mostly cuffed ETT’s.
· ETT sizing – Age/4 + 4 (uncuffed), Age/4 + 3.5 or 4 (cuffed)
IV fluids:
Intraoperative fluids?
Duration of surgery:
• Short surgery (<1 hour) + healthy child – do not usually require fluids if pre-operative fasting has not been excessive.
• Prolonged surgery (>1 hour) + unwell child/high risk such as blood loss/intra-abdominal surgery – should receive intravenous fluids.
How to calculate peri-operative fluid requirements:
Total fluid required =
fluid lost during the pre-operative fasting period + intra-operative losses + maintenance fluid requirement.
Maintenance fluids are calculated using the 4, 2, 1 rule (one method!)
• First 10 kg: 4 mL/kg/h (or 100 mL/kg/24 h)
• Next 10 kg: 2 mL/kg/h (or 50 mL/kg/24 h)
• Subsequent kg: 1 mL/kg/h (or 20 mL/kg/24 h)
(so a 10 kg child would have a maintenance fluid requirement of 40 mL/h
and a 25 kg child would require 65 mL/h).
Fluid boluses:
• Non-resuscitation: 10 mL/kg isotonic fluid (e.g. 0.9% Nacl)
• Resuscitation: 20 mL/kg isotonic fluid (e.g. 0.9% NaCl)
Emergencies:
Failed IV Access (after 2 x attempts) —> IO
Potential sites: Tibia, femur, sternum
Anatomical landmarks
• Tibia: medial side, 2–3 cm below the tibial tuberosity
• Femur – 3 cm above the lateral condyle
(these sites avoid epiphyseal growth plates and joint spaces)
Summary:
Always refer to your paediatric drug doses and calculate these beforehand whenever possible
Calculate your emergency drug doses for IV and IM
Know your ETT AND LMA sizing before any airway manipulation and what you would do in case of difficulties
Judicious fluid management is extremely important in paediatrics as it can be very easy to get carried away!
As always - paediatrics CAN and DOES come up in the Primary FRCA examination - know your key anatomical differences, resuscitation algorithms, drug doses and physiological differences well!