Bone Cement Implantation Syndrome - A clinical summary
Face to face exams are back ON!
Whilst we’ve transitioned to examining virtually over the last couple of years, it’s likely that many of you will feel apprehensive about going back to face to face examinations, particularly more physical aspects of the examinations such as resuscitation, simulation and physical examination.
This week’s blog post is on bone cement implantation syndrome. I’ve picked this as it is a topic less frequently discussed in OSCE textbooks and practice stations, however could quite easily come up as a critical incident in a simulation scenario, leading to a resuscitation scenario or even in a clinical VIVA.
Key points:
· Bone Cement Implantation syndrome (BCIS) can occur in any procedure but especially one that breaches the femoral canal such as
o IM nailing
o Cemented and uncemented hip implants
o HIGHEST RISK in frail patients undergoing CEMENTED HEMIARHTROPLASTY – significant cause of intra-operative morbidity and mortality (M&M)
· Most commonly occurs during cementing, prosthesis insertion or at tourniquet deflation
· Incidence: Approx. 25%
Cement indications:
· IM nailing
· THR (prosthetic)
Why cement ? long term survival much better with cement vs non cement
Risk Factors:
*pHTN = pulmonary hypertension
Predictors of 30 day mortality
· Age >85
· Male
· CCF
· Dementia
· Diuretics
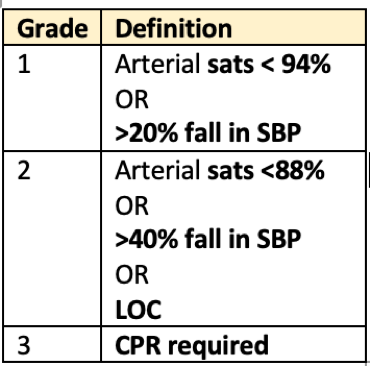
· BCIS grade 2 or 3
Proposed severity classification:
Related to predicted mortality
Advantages and Disadvantages of Cement:
Pathophysiology
Poorly understood - most supported model describes:
· Increased IM pressures —> cement, bone or tissue particles embolising to the RA —> increased pulmonary artery pressures (PAP) —> right ventricular failure.
o Absorption of mono methyl methacrylate, a component of cement may also contribute
· The following play a role:
o Inflammatory response
o Thermic
o Complement activation
o Allergy/anaphylaxis
o Subclinical pulmonary embolisms
- Peripheral vasodilation
- Reduced venous return
- Increase CO/SVR
Clinical features:
· Can present intra and post op (in a less severe form)
· Clinical hx and timing of cardiorespiratory collapse suggest BCIS
· Intraop signs:
o Hypoxia – decreased sats
o Hypotension, Sudden loss of arterial pressure
- Significant CVS compromise (can occur during preparation of femoral canal, during insertion of cement and/or prosthesis and when hip is reduced)
- Involves pressurised bone areas THR, TKR
o Pulmonary HTN
o Arrhythmias
o LOC
o Arrest
· Post op:
o Hypoxia
o confusion
How to minimise or prevent:
The University Hospitals Coventry and Warwickshire have developed excellent tools to assist teams in their recognition and management of BCIS. This role allocation table may be useful to your practice:
Management:
- Largely supportive – 100% o2, fluid resuscitation (guided by CVP), vasoactive/inotropic support
- Ensure invasive monitoring to help with early diagnosis and management
- ?HDU/ICU required
- Coventry curfew
Coventry Curfew:
This is a tool implemented by University Hospitals Coventry and Warwickshire in every trauma list and before every cemented hemiarthroplasty, the principles of which may again be useful to your practice in improving vigilance, rapid recognition and initiating management of BCIS.
References:
1. Safety guideline: reducing the risk from cemented hemiarthroplasty for hip fracture 2015 - https://doi.org/10.1111/anae.13036
2. http://intensiveclub.org/wp-content/uploads/2017/06/Bone-Cement-Implantation-Syndrome.pdf
3. Guideline for Management of hip fractures 2020