Regional Ready? (3 min read)
As we focus on how to improve the perioperative period for patients, regional anaesthesia has taken the spotlight.
Regional anaesthesia (RA) is for all anaesthetists, and I hope that the tips below will help you approach your blocks with more confidence! I looked at the newest BJA articles regarding safe practice, and have added in my own personal tips that I have picked up along the way!
Read till the end for the best way to answer ANY RA question in the OSCE!
Enjoy and I hope this helps you :)
1. Preparation
Stop before you block
sadly wrong sided blocks still occur, so don’t get caught out!
Remember, severe local anaesthetic toxicity is a risk
Be mindful of your dose calculations (!)
Safer to use ideal body weight in obese/pregnant patients
BE STERILE
Dedicated sterile, single-use transducer covers reduce the risk of transmitting infection between patients.
If you have NRFit connectors, use them!
in haste we can all connect the wrong syringe. the consequences are not worth it!
2. Navigating your Needle
In plane vs out of plane?
In plane can risk you damaging larger nerves, so if the out of plane approach is easier use it!
Watch your needle
The ultrasound image is effectively the width of a credit card
Your target should be perpendicular to the probe
In the words of my favourite consultant - “move the needle OR the probe, not both!”
Target tissue space not nerve space (!)
ultrasound offers a 2D image, so you might be in the perineural space without realising it.
Use the local to hydrodissect your way to the nerve space
remember you want to be pushing the nerve away from your needle.
use the LA to help you get to the nerve without damaging surrounding structures
it also makes the nerve “pop” so you can spot it easily
You don’t need circumferential spread
although we are often advised to get that “doughnut-like spread of LA around the nerve”, turns out whilst it does improve block onset time, there’s only one paper that shows that efficacy of the block is improved
multiple needle manipulations however = increased risk of neural trauma
weigh the risks vs benefits when trying to get “the perfect spread”
Use the volume that you need
Whilst the literature has said you only need a few mL for certain blocks, you need to be quite close to the nerve to obtain an effective block
why risk getting so close to the nerve?
as long as the area surrounding the nerve appears full - there’s no need for more volume
Use a peripheral nerve stimulator + ultrasound to minimise intraneural injection
Having recently used this technique, I can confirm it has made me so much more confident in obtaining a successful and SAFE block
it takes seconds to attach a nerve stimulator - so why not use it?
———————————————————————
How to answer ANY RA question you are thrown
When the examiner asks “how would you perform X block” make sure you have a structure.
The following framework can be easily adapted to any block, and makes sure that you don’t miss any critical steps that could lose you marks!
Preoperative - “what you need to remember before any block”
Pre-op assessment
Consent+ risks vs benefits
Weight + calculate Local anaesthetic dose (type, volume, concentration)
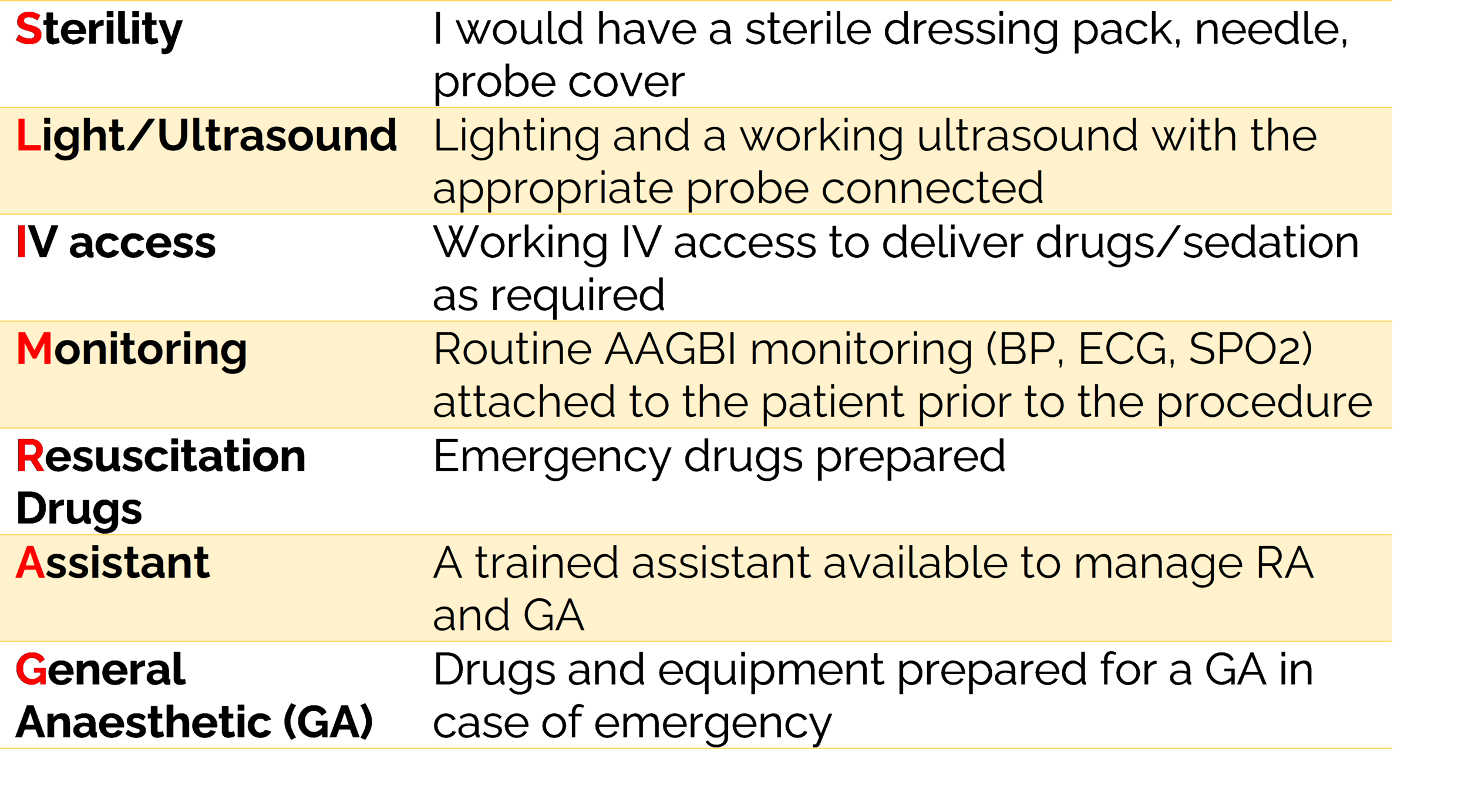
use SLIMRAG (below)
SLIMRAG - an acronym for preparation for RA
Intraoperative - “walk the examiner through the steps you would take in real life”
Position the patient
Locate anatomical landmarks
Clean the field with 0.5% chlorhexidine and allow to dry
(high/low frequency linear array) ultrasound probe with sterile cover and gel
STOP BEFORE YOU BLOCK
In/out of plane technique
Local anaesthetic to skin
Pass short bevel 50mm/80mm/120mm needle at an angle of X (directed cranially/caudally)
After negative aspiration, slowly inject X ml local anaesthetic confirming negative aspiration after every 5 ml injection (paying attention to injection pressure)
Postoperative - “How will you keep the patient safe afterwards?”
post op monitoring + follow up after 24 hours
protect limb from inadvertent harm (e.g. trauma, burns) and consider using protective slings/splints until return of sensation.
prescribe appropriate bridging analgesia
provide verbal and written advice on bridging pain relief to avoid a gap in analgesia and rebound pain
So there you have it! An amalgamation of all the top tips I have learnt (so far!).
Have more? Comment below and share them!
References
Topor B, Oldman M, Nicholls B. Best practices for safety and quality in peripheral regional anaesthesia. BJA Educ. 2020;20(10):341-347. doi:10.1016/j.bjae.2020.04.007
Abouzied T, Wilson A. Is accepted practice in regional anaesthesia really 'best practice'? BJA Educ. 2022 Mar;22(3):84-86. doi: 10.1016/j.bjae.2021.12.002. Epub 2022 Feb 2. PMID: 35211324; PMCID: PMC8847813.