Tracheostomies for the FRCA
With face-to-face exams being back, I’m predicting that the college would love to go back to certain stations which they were less able to convert to a virtual station!
How can tracheostomies feature in the Primary FRCA?
1. Technical skills – performing a tracheostomy change
2. Equipment – Identifying different types of airways, indications, contra-indications etc
3. Simulation – Emergency tracheostomy management
So, here is your masterclass to what you need to know for the Primary FRCA. And remember – knowing this well now, will serve you well for the Final FRCA as well!
I’ll approach this blog article in a systematic way demonstrating some of the ways in which questions could be asked. There is a key at the bottom of the article for some phrases written in short hand.
——————————————————————————————————————————————
What are the different types of tracheostomy techniques that can be performed?
Percutaneous = most commonly performed in ICU
Bjork flap = suturing an inverted u-shaped flap of trachea to the skin edge
Slit type = also known as a surgical tracheostomy
What are the different techniques for performing percutaneous tracheostomies?(1)
1. Percutaneous + multiple dilators
2. Percutaneous + single dilator (rhino)
3. Guidewire + dilating forceps
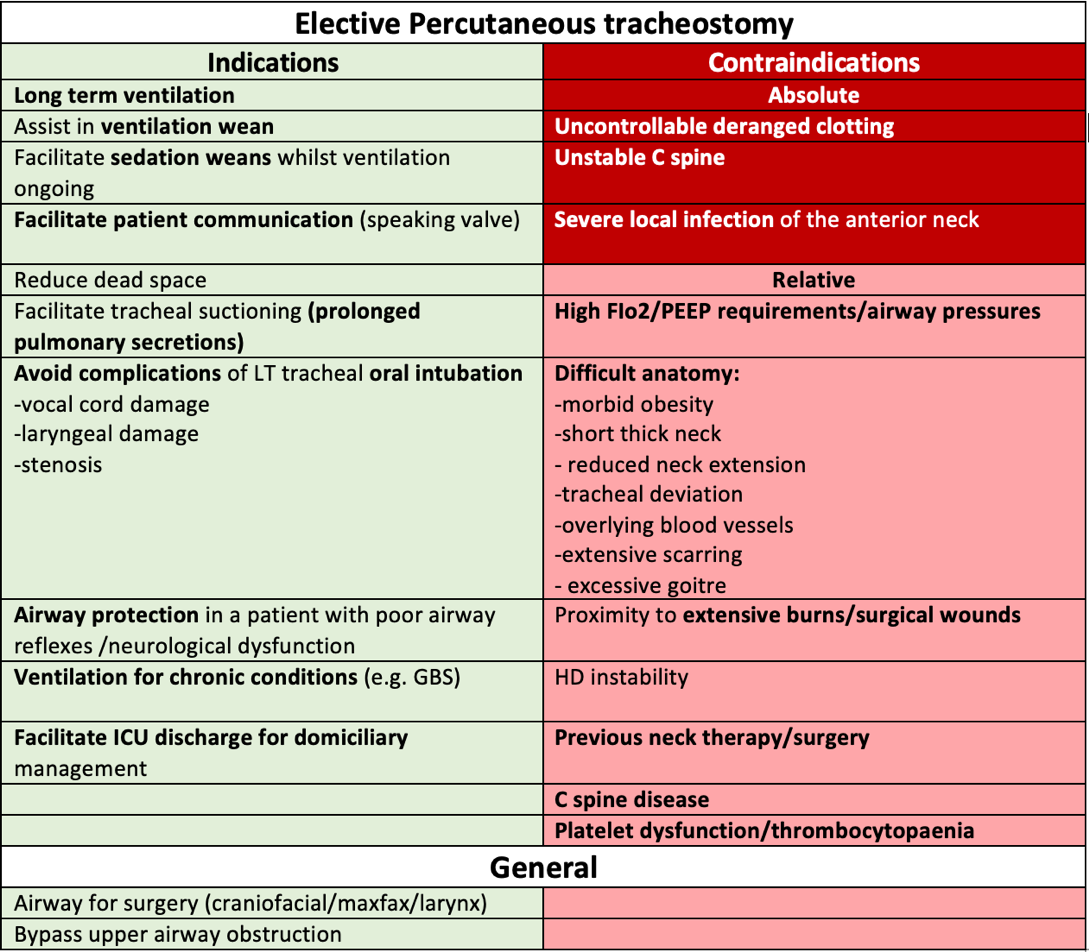
What are the indications/contraindications for a tracheostomy?(2, 3)
TOP TIP:
Pay attention to the wording of the question and give your BEST answers in relation to what is being asked. (you may be given a clinical scenario)
WHY:
1. If the answer isn’t on the mark scheme (even if its right/reasonable) you won’t get the mark!
2. Indications for elective percutaneous tracheostomies/surgical/emergency tracheostomies vary (although overlap) . The same will apply to similar questions.
What are the benefits of a tracheostomy?
1. Patient comfort
2. Patient communication
3. Less sedation required
4. Improved oral hygiene
5. dead space
6. airway resistance
7. glottic trauma
8. Bronchial toilet
What are the advantages and disadvantages of performing a percutaneous tracheostomy?
What complications can occur with a percutaneous tracheostomy? (2)
The table below has been described through a systems based approach which you might find useful.
What are your pre-operative considerations when thinking about performing a percutaneous tracheostomy on a patient?
Indications and contraindications (see above)
History:
1. Previous radiotherapy to the neck
2. C spine disease
Neck examination – the following may r/o complications/may make technique more difficult:
1. Short neck
2. Tracheal deviation
3. Aberrant vessel (can minimise risk using US)
4. Goitre
What steps are involved in your pre-operative preparation? (3)
At what tracheal level is a tracheostomy performed ?
Usually between the 1st and 2nd or 2nd and 3rd tracheal rings
What is the appropriate cuff pressure for a tracheostomy? 5
Between 20 – 30cmH20
How would you perform a percutaneous tracheostomy?
NB: this is a very simplified version, consisting of key points only. Techniques may vary by unit, clinician and tracheostomy device type.
TOP TIP:
YouTube is a great resource for insertion of tracheostomies!
How would you perform a tracheostomy tube change (without a bougie/guide wire) ?(4)
TOP TIP:
Click below to see a real life RCOA OSCE example -
How would you care for a (new) tracheostomy?
1. Ensure humidification of inspired gases
2. Regular tracheal suctioning
3. Fix securely to prevent accidental removal
4. Use a double cannula tube with inner tube to prevent blockage
What types of tracheostomy airways are there? (5)
Standard cuffed tracheostomy
Un-cuffed and cuffed fenestrated tracheostomy
Adjustable flange tracheostomy
Cuffed laryngectomy tube
Tracheostomy Emergencies
You are called by the nurse to ICU to review a patient with a tracheostomy due to a sudden desaturation. How would you proceed?
A question like this or similar to this is designed to test your knowledge of the National Tracheostomy Safety Project (NTSP) Emergency Tracheostomy Management algorithm. (1, 5)
Several algorithms exist for patent upper and non-patent (laryngectomy) upper airway management, and also for adult and paediatrics.
LEARN THESE – and you’ll be fine!
What airway information would you want before performing and emergency airway manoeuvre in a patient with a tracheostomy?
1. Date of insertion
2. Indication for insertion
3. Type (percutaneous/surgical/Bjork)
4. Type of tracheostomy + size of tracheostomy
5. Any previous difficulties in insertion or intubation
Summary
Hopefully by now, you should be a tracheostomy expert! I hope this article has increased your understanding of tracheostomies, and how to approach them in an elective, emergency setting, as well as exam setting! Take a look through the references below for further reading materials.
References
1. https://www.tracheostomy.org.uk
2. The Final FRCA Short Answer Questions – A practical Study Guide – Elizabeth Combeer
3. Guide to the FRCA Examination – The Final – 4th Edition – RCOA
4. RCOA example – https://www.youtube.com/watch?v=5BrPZEUz6zE (last accessed 12.4.22)
5. https://www.bjaed.org/article/S2058-5349(19)30125-8/fulltext
Key:
HD = haemodynamic
R/O = risk of
AoA = Association of Anaesthetists monitoring
# = fracture
PTX = pneumothorax
FB = foreign body
PT = percutaneous tracheostomy
PPE = personal protective equipment