MRI for the FRCA (reading time 10 mins)
This week’s blog post will go through Magnetic Resonance Imaging – another popular exam topic in both the Primary and Final FRCA!
Again, it will be in a similar format to previous blog posts, going through topics in a Q&A format to give you an idea of what can come up in both an OSCE or VIVA setting
We’ll discuss:
Patient Selection
MRI principles
Key facts about MRI
Contraindications to MRI
MRI hazards and safety
intraoperative-MRI (i-MRI)
Summary
—————————————————
1. Patient selection
What types of patients might require anaesthetic input?
This list is not exhaustive, but should give you a good idea.
- Patients unable to lie still:
o Small children/infants
o Movement disorders
o Positioning limited by pain
- Individuals with learning disabilities
- Individuals suffering from claustrophobia
- I&V patients/ICU patients
- Patients having surgery with intraoperative MRI
2. MRI Principles
Can you describe the basic principles of MRI?
The college answer…buzz words here are EVERYTHING
- Non ionising radiation
- Uses interaction between static magnetic field (MRI magnet) and the magnetic field that arises from atoms.
- Patients are placed within a strong magnetic field (0.5 – 3 Tesla)
- Some atoms with an odd number of protons (such as hydrogen) have an asymmetrical spin
- When an external magnetic field is applied:
o the protons align either almost parallel or opposed to the field
o the protons wobble in their axis of spin at a frequency proportional to the field strength – this is called precession
- A radiofrequency (RF) current is then applied at the frequency of the atoms precession causing the protons to flip out of alignment and absorb energy
- RF current is switched off – protons flip back and release radio wave energy (they relax with different time constants in different tissues)
- Energy is detected and images are generated
- Secondary gradient fields (static fields with small dynamic gradient fields) allow spatial localisation by altering the precession frequency between tissues, and allow signals to be localised.
HOT TIP:
Or check out this YouTube video below which I have found very useful in getting to know the basics:
3. Key facts about MRI
In what unit is the magnetic field of an MRI measured in?
Tesla
1T = 10,000 gauss – MRI field strength is usually 0.5 – 3 T
Earth’s magnetic field = 0.5G!!
What is T1 and T2 weighed imaging?
T1 – used to identify grey-white matter contrast
Fat is bright/white
Water is dark
T2 – used to identify tissue oedema
Fat is dark
Water is bright
What is gadolinium?
Gadolinium – is a contrast agent which can alter the relaxation rates of hydrogen nuclei
What are the side effects associated with gadolinium?
- N&V
- Pain on injection (mild)
Rare but serious… What are the two main adverse effects of gadolinium-based contrast agents?
- Anaphylaxis
- Nephrogenic systemic fibrosis – caution in renal impairment
o Avoid contrast if eGFR <30ml/min
o Do not repeat contrast within 7 days
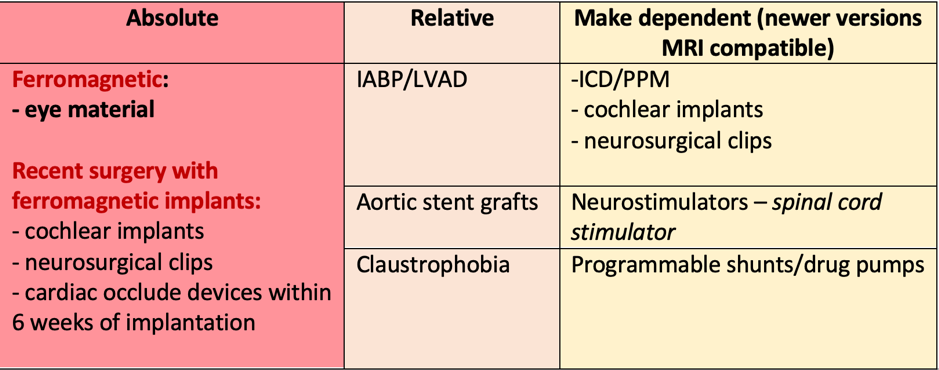
4. Contraindications to MRI
What are the contraindications to MRI?
5. MRI hazards and safety
Learn these symbols!
Definitions:
1. MR Safe: can be used in any MR setting – no MR-related hazards to patients or staff
2. MR conditional – No MR-related hazards to patients or staff when used in MR setting under specific conditions – e.g. static field strength, rate of change of magnetic field.
MR unsafe–hazardsrelated to patient or staff– CANNOT BE USED
What precautions should you take while a patient is having an MRI scan/ to minimise the risks associated with MRI?
SAFETY:
People
· Ensure checklist complete for patient/staff
· Ear protection - staff and patients (awake or anaesthetised) should wear ear plugs – sound range of MRI 65 – 130dB! (normal conversation is about 60dB)
· Avoid taking any ferromagnetic objects into the room; pens, phones, stethoscopes
· Ensure clothing non-ferromagnetic (e.g. some sportswear contains silver fibres)
· Pregnancy – avoid in the 1st trimester- unknown effects
Equipment:
· Non-ferrous trolley before entering MRI scanner
· MR safe ventilator/anaesthetic machine
Environment:
· Ensure oxygen sensors are present on the walls - quenching refers to helium escape when the magnet is shut down in an emergency. Liquid helium expands to gas and vents quickly via quench pipe. If room vents are blocked, helium will fill the room and displace O2 resulting in a hypoxic environment.
· Ensure familiarity with environment/equipment/emergency kit prior to commencement
PRACTICAL CONSIDERATIONS:
Patient:
· Pilot balloon of ETT may contain ferromagnetic material – secure AWAY from site of scan
· Risk of hypothermia – the helium is kept cool at close to -240 degrees - patients may need to be warmed
· Warn patient re. :
o High strength Tesla can induce nausea/vomiting
o Time-varying magnetic gradient fields – can stimulate peripheral nerves or muscle cells à twitching
· Airway inaccessible during the MRI scan – ensure that it is secured in place
· Remote site anaesthesia and its challenges
o Ensure senior support available
Equipment:
· Check all equipment is MR safe or MR conditional
o Ensure all equipment not ferromagnetic – special trolleys, gas cylinders removed
· Check sufficient length in monitoring equipment + breathing circuit
o Long IVF lines for MRI
o Long sampling lines – e.g. arterial line, capnography – caution when interpreting results as delays/errors (damping) can occur.
· MRI safe or conditional infusion pumps
· Ensure all monitoring is visible
o Telemetric to facilitate presence in screen control room, reduces risk of failing to notice abnormalities
· MRI safe equipment should be clearly identifiable
General precautions to minimise risks in MRI:
Equipment check
· Remove drug delivery patches (may contain metal) – risk of burns
· Padding over RF coils – prevent direct contact between patient + RF coils
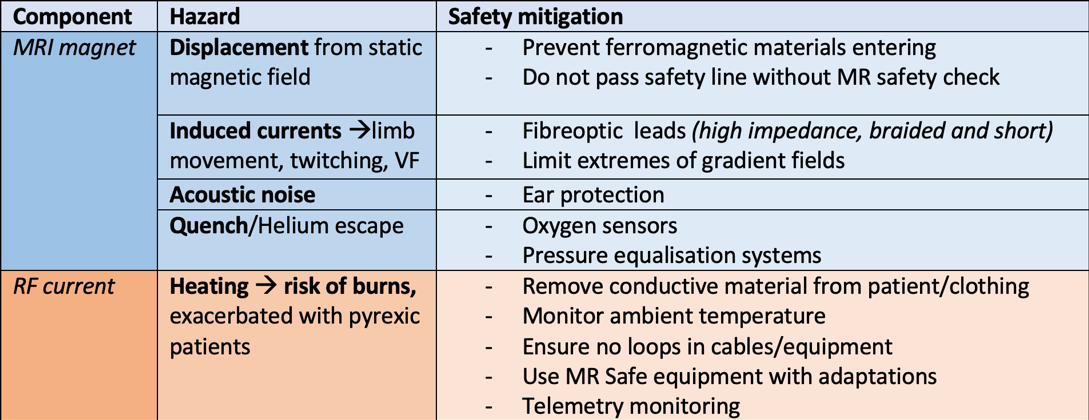
What are the hazards of MRI and how do we mitigate these?
Think of this in terms of each major component and the hazards it poses
How do you prevent burns caused by monitoring equipment in the MRI scanner?
· Use only MR safe or MR conditional that is deemed appropriate for scanner
o Nylon NIBP connectors
o Graphite ECG electrodes – placed in a narrow triangle on patients chest to minimise impedance.
o Non ferromagnetic monitoring e.g. skin temp strips
· Check all equipment prior to use – intact, no breach in insulating surfaces that might risk metal touching skin
· Cables and minimising risk of induction currents which could potentially cause burns:
o Fibreoptic (ECG leads/pulse ox) Note – can cause signal distortion; filters used to improve.
o Insulated
o High impedance and short/braided e.g. ECG leads
o Ensure correctly applied ECG electrodes – minimise impedance
o Should not be directly touching the patient – padding placed between cables and patient skin
o Should not cross/coil/loop each other – induction currents can result from capacitance coupling.
o Run down the middle of the patient/scanner, not at the outer edges close to the RF coils. (Padding should be placed between patient and RF coils)
o Telemetry monitor to eliminate risk of induction currents in connecting leads
What adaptations are there in monitoring and equipment?
Monitoring
- All monitoring should be in the control room and mostly telemetric (AoA recommended)
- Capnography – side stream analysers used as in line samplers overheat.
o Caution as side stream can cause delays in reading due to the length of sample tubing
- Fibreoptic pulse oximetry (see above)
- Graphite ECG electrodes – placed in a narrow triangle on patients chest to minimise impedance.
- ECG – Monitor V5 and V6 as furthest from aortic flow induced voltages therefore reducing artefact.
o Monitor for ST/T wave changes which could resemble pericarditis or hyperkalaemia
o Cardiac motion artefact reduced by ECG gating – when a scan is triggered to gain information during a specific portion of the cardiac cycle
- Nylon NIBP connectors
- Non ferromagnetic monitoring e.g. skin temp strips
Equipment
- Non MRI safe/conditional equipment kept outside scanning room or outside specified G line
o Note – long tubing therefore increased risk of disconnection
- MR compatible piped gasses (non ferromagnetic, usually aluminium)
- All gas cylinders MR compatible
- Airway equipment – MR compatible laryngoscopes, ET tubes, LMA’s, ventilators, infusion pumps, suction, patient trolley
6. Intraoperative - MRI (i-MRI)
Name some indications for intra-op MRI?
1. Excision of tumours
2. Epilepsy surgery
3. Insertion of deep brain stimulator (DBS)
4. Thermal ablation
5. MR angioplasty
6. Biopsies – liver/breast
What are the advantages and disadvantages to intra-op MRI (i-MRI)?
What are the anaesthetic concerns unique to the management of a patient undergoing surgery using i-MRI?
1. Prolonged operating/anaesthetic time
2. Multiple transfers - require several trips between theatre and i-MRI to complete surgical margins
3. Access limited – during positioning or when in the scanner
4. Safety
a. Displacement of tubes/lines
b. potential for MRI unsafe surgical/anaesthetic equipment to be moved into magnetic field due to error
7. Summary:
Hopefully you’re an MRI pro by now - knowning the principles, common indications/contraindiciations and everything about MRI safety and hazards, as well as its use in the intraoperative environment. Check out the references below for further reading.
References:
https://www.bjaed.org/article/S2058-5349(18)30018-0/fulltext
The Final FRCA Short Answer Questions – Elizabeth Combeer
Guide to the FRCA examination – the Final. Royal College of Anaesthetists