Resuscitation: Special Circumstances Part 2
Part 2 of our resuscitation series looks at resuscitation in trauma and how our management approach differs in the ED, management and cardiac arrest setting.
In this week’s blog, we will cover the following:
Key definitions
Approaching the trauma patient
Management principles
Traumatic Cardiac arrest
—————————————————————
1. Key definitions
Major trauma:
Injury or combination of injuries that are LIFE THREATENING and could be life changing because it may result in a long term disability i.e. loss of limb
Injury severity score >=15
Major trauma centre (MTC):
Multispecialty hospital with facility to manage all trauma patients. Consultant led 24/7, 365 days
Major trauma unit:
Facility to stabilise major trauma for transfer to MTC. i.e. unable to provide immediate specialist care for major traumas e.g. gunshot wounds
Damage control resuscitation: (DCR)
DCR is the principle haemostatic resuscitation – avoid excessive crystalloid and replace with guided blood products (blood, FFP, use ROTEM) External pressure
Haemostatic gauze
Tourniquets
Pelvic binder
Permissive hypotension
Avoid lethal triad
CRASH 2 trial: Early tranaxemic acid (TXA)
Loading dose: 1g over 10 min, followed by 1g over 8hr
TXA safely reduced the risk of death in bleeding trauma patients
CRASH 3 trial:
Early TXA (within 3hr) did not result in a significant reduction in TBI associated death at 28 days, however it also does not appear to cause harm.
Damage control surgery (DCS)
Damage control surgery (DCS):
· DCS is the management (3 phases)
· Phase 0 – Initial resuscitation and restoration of physiology
o Phase 1 – abbreviate laparotomy
o Phase 2 – stabilization on ICU
o Phase 3 – Further exploration
Major haemorrhage:
· >1 circulating blood volume in 24h. (approx. 70ml/kg or approx. 5L in 70kg adult)
· 50% total blood volume loss in <3h
· Bleeding >150ml/min adults
Massive transfusion:
· Complete replacement of circulating volume in 24h
· 50% blood volume transfused in 4hr
· 10 units given in 24h
2. Approaching the trauma patient.
Your first assessment of the trauma patient is likely to be in the Emergency Department.
General principles:
ATLS approach, call for help
Primary survey – cABCDE + Ruling out/looking for immediate life threatening injuries: ATOM – FC
A – Airway obstruction
T – tension pneumothorax
O – open pneumothorax
M – massive haemothorax
F – flail chest
C – cardiac tamponade
Key points of difference in your cABCDE approach include:
cA: (c/spine + Airway)
MILS
Assess for severe facial trauma, blood
?need for intubation – predict difficult airway!
Maintain C spine precautions until cleared via guidance (see below)
B:
100% oxygen.
If intubation required - RSI – trauma, pain and opiates are all associated with delayed gastric emptying
Cardio stable induction to minimise pressor response. Choice depends on preference but generally opiate, ketamine, rocuronium.
Remember lung protective + neuro protective ventilation
C:
IV access, fluid warmer
Resuscitate - IVF + blood products
Bloods, ABG, lactate, BC, ROTEM/Haemacue/Transfusion triggers , rapid infuser
FAST SCAN
HAEMORRHAGE ? Major haemorrhage protocol AND…
External pressure
Haemostatic gauze
Tourniquets
Pelvic binder
CRASH2: TXA
Rapidly reverse anticoagulation in patient who have major trauma with haemorrhage
Warfarin - vitamin K, Prothrombin Complex Concentrate (PCC)
Dabigatran - idarucizumab (aka Praxbind)
Apixaban/Rivaroxaban - Andexanat alfa (aka Ondexxya)
Discuss with haematologist if < 16 years or if on any other agent other than warfarin
D:
Pupil assessment
GCS assessment/AVPU
Don’t forget glucose!
E:
Assess abdomen, pelvis, long bones
Altered pharmacokinetics likely. SENIOR discussion early
Use the following mnemonic for a quick history:
A – allergies
M – Medications
P – Past medical history
L – Last meal
E – Events leading up to the presentation
3. Management principles:
· Avoid lethal triad:
1. Hypothermia
2. Acidosis
3. Coagulopathy – Keep fibrinogen >2
· DCR and DCS (see above)
· Aim for radiological imaging if sufficient time/patient is stable
o See NICE guidance CG176 on CT head/C spine imaging indications
o See NICE guidance CG39 on Major trauma: Assessment and initial managent with regards to whole body CT
· C spine clearance
o Assess risk according to Canadian C spine rules – high, low or no risk (caution – applying these rules to children can be difficult and the child’s developmental stage should be taken into account)
o C spine can be cleared clinically or radiologically as determined by risk stratification
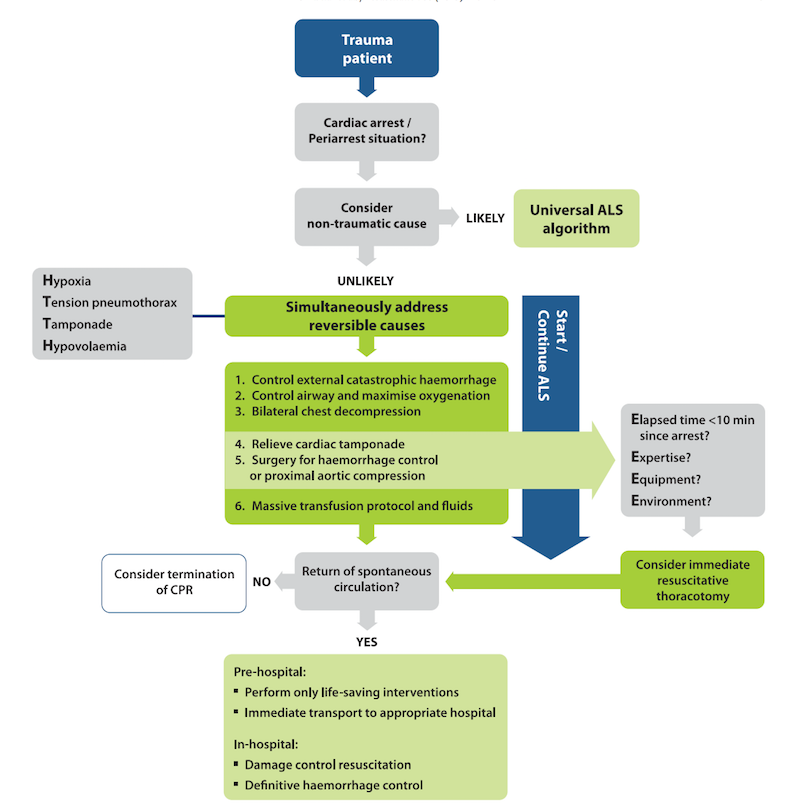
4. TRAUMATIC CARDIAC ARREST (TCA)
· Common Causes: hypovolaemic shock, obstructive shock, neurogenic shock
· Focus: immediate, simultaneous treatment - Chest compressions MUST NOT DELAY treatment of reversible causes.
· HAEMORRHAGE ?
o External pressure
o Haemostatic gauze
o Tourniquets
o Pelvic binder
· FAST scan
· Consider LIFE SAVING interventions
o Haemorrhage control incl pelvic binder
o Optimise oxygenation/ventilation
o Vascular access
o Rapid warmed blood/blood product transfusion
o Bilateral thoracostomies
o Resus thoracotomy – especially in penetrating trauma
Take a look at the ERC algorithm for the management of Cardiac arrest 2015:
References/Further reading:
https://www.nice.org.uk/guidance/ng39
injurieshttps://www.nice.org.uk/guidance/ng39/chapter/Recommendations#immediate-destination-after-injury
https://www.resus.org.uk/library/2021-resuscitation-guidelines/special-circumstances-guidelines
https://rcem.ac.uk/wp-content/uploads/2021/10/RCEM_Traumatic_Cardiac_Arrest_Sept2019_FINAL.pdf
https://www.resuscitationjournal.com/article/S0300-9572(15)00329-9/pdf